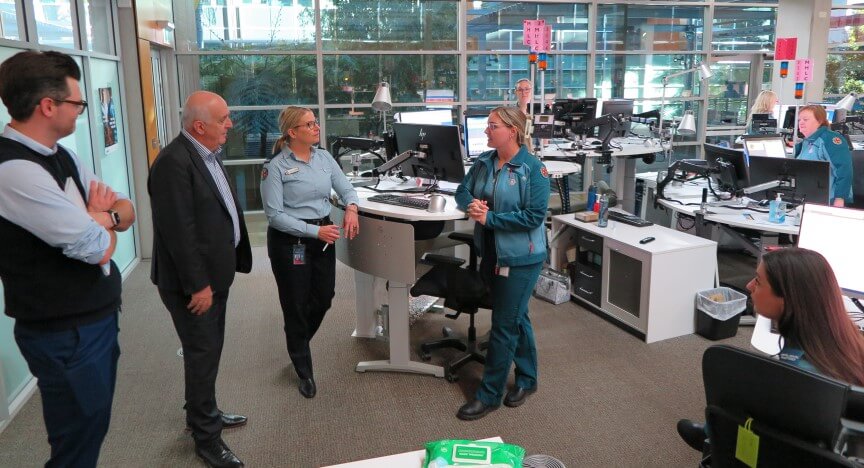
How Queensland Ambulance Service has adapted its response to a steady increase in calls from vulnerable people was in the spotlight this month when Queensland’s Mental Health Commissioner Ivan Frkovic visited the Kedron Park headquarters.
The Commissioner and the Commission’s Suicide Prevention team met QAS’s Mental Health Response Program Director Sandra Garner and Mental Health Liaison Service (MHLS) Clinical Manager Steve MacIntyre to learn more about our tailored approach to responding to vulnerable and complex patients, before visiting the teams working in the Operations Centre.
Sandra said the QAS’s Mental Health Liaison Service (MHLS) in Kedron Park’s Operations Centre began with five clinicians in 2020 and has since grown to a team of 30, operating 24 hours a day, seven days a week.
“Over the last few years Triple Zero (000) calls from people experiencing a mental health crisis have increased from 100-120 per day before COVID19 to 150-180 calls per day,” Sandra said.
“And sadly, we receive between 10 and 20 calls a day from people either experiencing suicidal intent, or who are attempting to end their own life.”
Steve said the MHLS was developed to ensure people experiencing a mental health crisis were responded to in a timely and appropriate way.
“Our team provides support, advice and assistance to frontline staff as well as directly to people experiencing a mental health crisis who call Triple Zero (000),” he said.
“On average the team reviews around 350 jobs and speaks to around 250 people each day.
“This is the busiest team I’ve ever worked in.
“We have a direct impact on people experiencing a mental health crisis – we save lives every day – whether it’s by keeping a Triple Zero (000) caller talking to us until paramedics arrive, or by getting help to them sooner,” Steve said.
The Mental Health Commissioner said it was great to see some of the work underway at QAS to enhance and improve responsiveness and support for people in crisis, and ultimately help save lives.
“Queensland has the second-highest rate of suicide in the country, but encouragingly, we are seeing a downward trend beginning to emerge in the number of suicides, both in number and per capita terms in Queensland over the last three years,” Ivan said.
“To reduce and prevent suicide in Queensland, requires a whole-of-government and whole-of-community approach to people experiencing suicidality or distress.
“Every touch point provides an opportunity to engage and encourage help seeking.”
Sandra and Steve also discussed why the Social Worker team was integrated into the Clinical Hub’s multidisciplinary team and how the team’s knowledge and skills have benefited not only their colleagues and on-road staff, but also overall patient care over the last year.
“Our frontline staff identified a growing cohort of vulnerable patients in potentially unsafe environments,” Sandra said.
“We were seeing a rise in paramedics calling with safety concerns for children, people with a disability and the elderly.
“Our paramedics see people in their own environment and are welcomed into people’s homes no matter what state they’re in, which is a rare opportunity.
“So, we now have a team of social workers who can provide our paramedics with support and advice at the scene or on the phone who can provide follow up assessment and referral options outside the single episode of care.
“They can also bring in extra supports, enabling vulnerable people to stay in their homes rather than sending them to hospital, which is a win for families in need and it gives our paramedics the peace of mind knowing we’re following up on patients they’re concerned about.”
The team also discussed its plans to develop a safe and appropriate response to frequent calls from people who are vulnerable with complex needs.
“We know hospitals are the best place to be for illness, injury and trauma; although this can be busy and overwhelming for a person who needs extended care,” Sandra said.
“The benefits to having access to appropriate assessment, care and referrals closer to home, even over the phone, have been recognised widely and people who receive our services are grateful for the experience.”
Ivan said it was wonderful to visit the QAS team and hear firsthand about their multi-disciplinary team, and how the scope of their role has changed from not only addressing the presenting problem, but taking a more wholistic approach to helping people to navigate the system and get the support they need.
“System reform is not just about re-designing old services, it’s also about developing new and innovative ways of working that bring the system forward,” he said.