
Ask any patient our Falls Co-Response teams have responded to over the last year, and they’ll tell you what a positive experience they’ve had.
The Falls Co-Response Program partners a paramedic with an Allied Health Professional (AHP), either an occupational therapist or a physiotherapist to respond to people who have fallen and have either minor or no significant injuries.
The teams operate from 6am-6pm, seven days a week with the aim of ensuring patients who have fallen are responded to and are assessed sooner, while at the same time, the use of referral and appropriate treatment pathways.
QAS Insight spent some time out on the road earlier this month with one of the program’s first crews based at Durack Station.
Just after dawn in early October, I arrived at Durack Station, ready to hit the road with one of the original teams recruited last year to the Falls Co-Response Program pilot.
I was to meet ACPII Paramedic Natalie Ballard and Queensland Health’s Metro North and Metro South Senior Physiotherapist Natalie Davis.
As “The Nats” nattered while completing final checks of their kit and truck for the day, I took the time to have a look at the van, its set up, and learn more about the team itself.
The team’s vehicle is a QAS-branded people-mover without lights and sirens, but with extra seats and luggage space for medical kits, lifting devices and a printer, along with a folder of helpful information sheets for patients.
Paramedic Nat said these vans were not equipped with lights or sirens so responding and/or transporting Code 1 was not possible.
Nat grew up in Mareeba, Far North Queensland.
“I’d wanted to become a paramedic when I left school, but the local station’s Officer in Charge (OIC) who knew us told Dad I should go and do something else for a while first and then return with some life experience,” she said.
Nat took on this advice and returned to her first career choice after moving to Brisbane and completing a social work degree at university and working in the industry.
She then applied to join the QAS’s ranks and said after more than 20 years as a paramedic, she hasn’t looked back.
“I absolutely love what I do – I wouldn’t have it any other way,” Nat said.
Meanwhile, Physio Nat grew up in a medical family in Essex, UK and moved to Australia four years ago.
“As a youngster I was pretty sporty, which of course meant injuries,” she said.
“My parents knew physios who’d treat me and there was one whose knowledge and communications skills inspired me.
“After school, I decided to complete a degree in Sports Therapy, quickly followed by completing a Masters in Physiotherapy.
“As a junior I did my NHS rotations, and gained invaluable experience working in women’s health, complex medicine, Neurology and intensive care units (ICU).”
Nat later secured a senior position at King’s College Hospital, in London, which introduced her to working in a community setting in addition to the Emergency Department (ED) and Major Trauma and Orthopaedics, bringing with it the variety she really enjoyed.
Her decision to move to Australia stemmed from the combination of trips to visit family friends in Australia and professional development opportunities.
“A lot of research comes out of Australia, so I felt working here could provide good clinical experience and professional development and having found this role in the Falls Co-Response team – I love it,” Nat said.
Working in a co-response team has become a new normal for Para Nat, who’s also worked in the Mental Health Co-Response teams.
“In this job you have to be flexible and adaptable, use your initiative, identify when things need to be done and do them, and you need to be able to read the room a bit as well,” she said.
“This is where our Allied Health team members are so valuable – they’re really motivated and keen to get in and give us a hand, they possess a fantastic work ethic, they’re senior, experienced clinicians with a wealth of specialised knowledge and skills and are fantastic to work alongside.
“Quite simply, they make my job easier and make coming to work a joy.”
Para Nat scanned iROAM for potential falls patients to respond to while Physio Nat checked in with the Clinical Hub where another AHP was embedded.
She described the inclusion of AHPs in the Clinical Hub as a “game changer”.
“This inclusion has helped raise staff awareness of our teams, and they act as an extra set of eyes watching over the jobs too,” she said.
The embedded staff contribute to the Clinical Hub’s brains trust, not only acting as a resource for on-road paramedics but are also able to speak directly with lower acuity Triple Zero (000) callers about their emergency.
Back on road, the Nats said the falls teams mostly attend to patients living independently rather than those in residential aged care with registered nurses on staff.
“We’ll often self-attach to the jobs,” said Para Nat.
“We’ll look at a patient’s age, whether they’re still on the ground or not, are experiencing any pain, whether any injuries have been identified which might necessitate a hospital assessment, whether there’s anyone around them to provide extra support and transport if they need it, and we’ll also consider their weight and mobility level as we don’t have stretchers in our vans, just passenger seats.
The Nats said the number of falls jobs a day will vary as does the ratio of falls to medical jobs, but they would often have four to five patients a day.
One of the patients we saw this day was an elderly man who had fallen in his bedroom and was unable to get back on his feet – and according to the Nats, a typical patient they would respond to.

His wife had called Triple Zero (000) and then made him comfortable on the floor while they waited for us to arrive.
The Clinical Hub Falls Responder had already completed a call back, identified this as a suitable case and provided the on-road team with relevant information.
While on our way, the Nats discussed this patient’s situation and the equipment we’d need to take inside with us.
Before we arrived, Physio Nat also had the opportunity to review the patient's medical history on iEMR and The Viewer, which supports them both in understanding a patient's health background.
The teams carry a range of lifting devices including the Raizer II, Camel, Elk, and HoverJack, to ensure they can lift patients of all sizes out of most situations safely.
Paramedic Nat said the team always ensured the closest parking space was kept free to ensure easy access in case an acute team was needed.
Margo, the patient’s wife greeted us and showed us through to her husband, Harry.
Paramedic Nat said she was relieved to see Harry looking alert in the couple’s bedroom on the timber floor.
There was no clutter around him, and access was easy as the bed could be moved.
While Paramedic Nat checked Harry’s vital signs she asked him how he’d ended up on the floor.
“Harry was walking into the bedroom, has tried to grab hold of a cupboard to stabilise himself, and his hand has slipped off, he’s lost balance and fallen landing on his buttocks with a head strike on the timber floor,” Nat said.
Once the initial joint assessment established his vitals were unremarkable and Harry had no significant injuries or pain, the Nats assembled a lifting device called The Raizer, which was placed under him while he lay on the ground before it slowly folded in to become a chair, supporting while lifting Harry into a seated position.
Now upright, the team again checked his blood pressure, and dressed a skin tear on his hand.
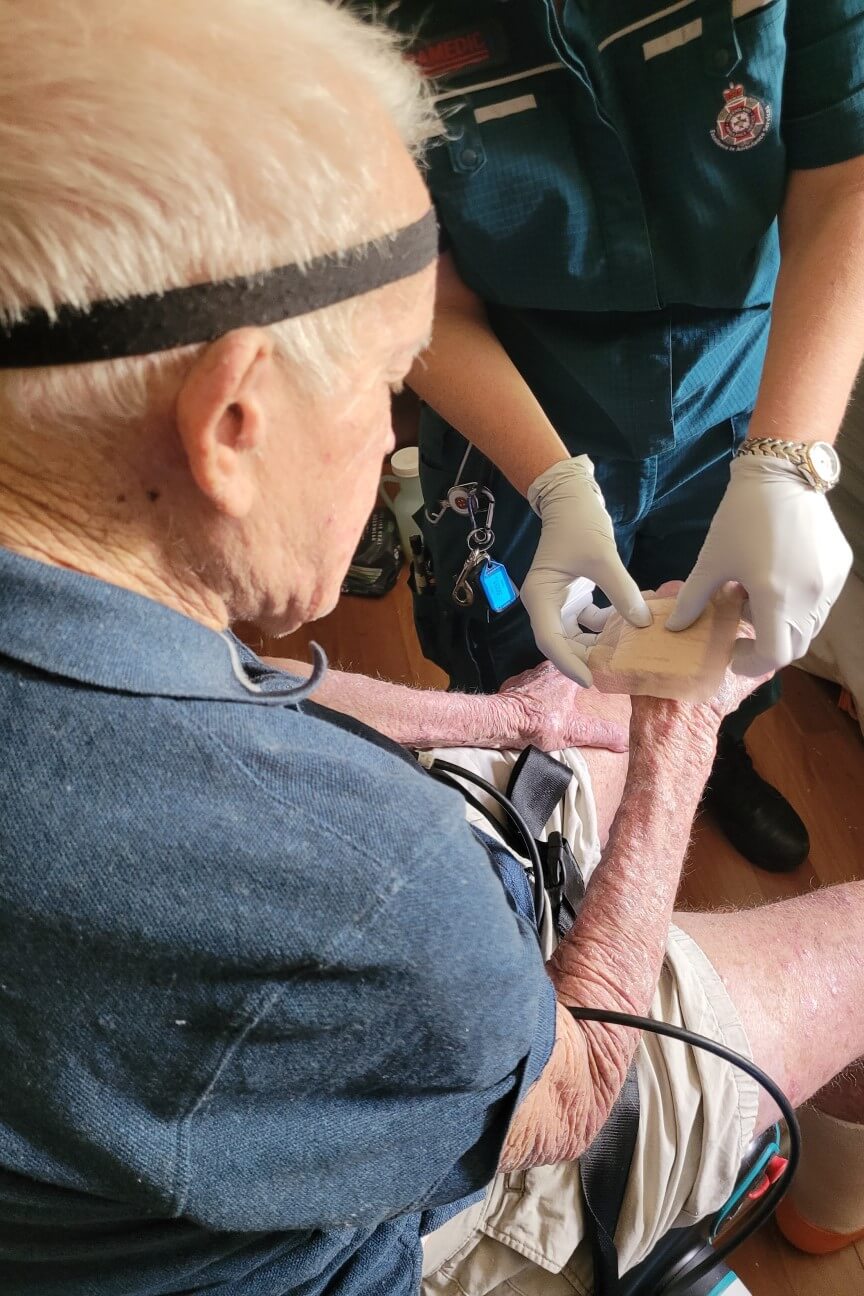

“Once I’ve finished my checks and am satisfied Harry’s stable, we’ll swap over so Nat can complete her physical musculoskeletal head to toe assessment and review the way the home is set up, what supports they have in place, and see what we can put in place or organise to help keep them at home safely,” said Para Nat.
Next, Physio Nat trailed Harry standing to his mobility aid and once deemed safe to do so, walked him from the bedroom to the lounge where he could sit in his armchair more comfortably.
“When they're on the ground for a while, they're going to be stiff, and it's going to take them a while to get back into their normal movement patterns, but we were definitely concerned about Harry’s mobility and safety at home,” Para Nat said.
Physio Nat said in fact her assessment actually begins as the team arrives at a house.
“I take into account the suburb which determines which referral pathways may be available to utilise, and the type of house they're in.” she said.
“I’ll be looking at the home’s accessibility, externally and internally whether it includes steps, ramps, rails, or any uneven surfaces.
“In this instance, I noted on entry a small threshold step navigating on shiny, slippery tiles and a steep, slim set of stairs with a rail up only one side, leaving the other side completely open – a falls risk even for us.
“Alongside this I noted the small threshold step into the toilet and bathroom which had some handrails, a slippery timber bedroom floor and quite a high-set bed, easy to roll or slip off, which moved easily despite the floor stoppers.
“I ensured I spoke with his wife Margo, about Harry’s health and mobility from her own perspective too.”
Harry was asked to stand and sit a few times while The Nats watched him closely.
While he chatted about his life, Physio Nat continued Harry’s functional assessment, putting him through his paces, testing his ability to move around the house and his ability to respond to higher risk situations like using the stairs and getting something from the fridge for lunch.


“He had quite a poor walking pattern, was stuck in a flexed posture with bent knees, had poor use of his walker, along with lower limb swelling.
“Overall he appeared to have multiple risk factors that would place him at a high risk of further falls” Nat said.
There were times during his assessment when we would see Harry starting to sag at the knees.
Meanwhile Paramedic Nat stayed with Margo to find out more about the couple’s home life and was told Margo had been Harry’s primary carer since his first stroke 40 years ago.
“I think there's a lot more going on with Margo, she seemed overwhelmed, looked tired and commented several times about Harry’s behaviour becoming increasingly challenging,” Nat said.
“Being a full-time carer can be exhausting and they also need support.”
With Harry’s assessment complete, he returned to his lounge chair with Physio Nat, joining Margo and Para Nat to discuss options with the couple.
The Nats discussed Harry’s bilateral lower leg swelling and longstanding leg ulcers Margo had dressed, as well as a nasty, lingering sore on his bottom and suggested with the couple’s consent, they would arrange a referral for a review from a range of professionals including nursing, OT, and PT to visit using Metro South’s Multi-disciplinary hospital Avoidance and Post-acute Service (MAPS).
This program could also link in a social worker to help Margo access a local Justice of the Peace (JP) to witness signatures for an Enduring Power of Attorney (EPOA) she’d needed to organise for some time.
The Nats left Margo with information and contact details for accessing extra support through Carer’s Gateway and a My Aged Care advocate to help her navigate the system to help the fiercely independent patient remain in his own home more safely.
“Whilst talking to Margo, I understood that she felt she had limited support around her and was concerned for Harry’s deterioration in function and cognition.
“While Margo was desperately trying to help, she also received a lot of reluctance from Harry to accept support.
“If we can set up that safety netting around Harry and advise of some better supports for Margo, that will ensure the foundations are in place for the support to be scaled up as Harrys natural trajectory of the aging process continues over time.”
Physio Nat completed her documentation and referral to the MAPS team following the review.
Paramedic Nat said the Allied Health team members’ knowledge and skillsets complemented their paramedic colleagues’ enormously.
“I love this co-response concept as it gives us a far broader scope of what we can assess and achieve in a prehospital setting when you have a vulnerable patient in their own environment,” she said.
“Our patients overwhelmingly love and appreciate this service because we take our time to assess them thoroughly, to listen and understand them so we gain an accurate picture of the issues they’re dealing with, so we can come up with a more holistic plan.
“For me as a paramedic, I also feel much more confident to leave my patients in their own home because I have these exceptional teammates with their specialised skill sets and knowledge backing my decisions.
“Our patients see a paramedic and invite us in to check them over and once you start chatting you can say, ‘Hey it’s your lucky day because I’ve got my colleague Nat here who is actually a Physio (or OT depending on which clinician you are working with on the day) and can see what she can do to make your life easier and safer’.”
Physio Nat said early intervention means the OTs and PTs can identify risks, provide falls prevention advice/strategies and action onward referrals appropriately to hopefully prevent more serious, life-changing events that can occur following a fall.
"As health professionals, we have a duty of care to our clients and should always respect the wishes of an individual – and in our assessment we always aim to optimise their quality of life by providing these specialised joint assessment and links in with support," she said.
“Using our combined knowledge and skillsets, our aim is to ensure patients who’ve had a fall are given the chance to remain at home as deemed appropriate following our assessment and are not just sent to hospital simply to keep them safe.
“We have the combined ‘tool kit’ to instead link these patients in with the supports they need to remain living in their own homes independently and safely, with a reduced falls risk, for as long as possible.
"It's so valuable being able to work alongside the paramedics as many of our patients are quite elderly with pre-existing medical conditions.
"It's great they can check the patient over for any new injuries but are also able to consider the impact of their other health issues and medications.
"We have an amazing ever-growing list of pathways we utilise other than hospitals, including teams like the Queensland Health-provided Community Health services, Mater at Home Direct, GP’s, Urgent Care Clinics and Satellite Hospitals."
The program was awarded this year’s Council of Ambulance Authorities (CAA) Excellence in Patient Care and also took out the overall Star Award.