
At the northernmost tip of Australia, Cape York is a beautiful, yet challenging landscape for the Queensland Ambulance Service to navigate.
It is a large, but remote land mass, covering more than 128,000km2 and has just 14,000 people living there, with 62 per cent of the population identifying as Aboriginal or Torres Strait Islander people.
In 2023 the Cape York Project was born, recognising the challenges the QAS faces delivering services to this area, but with the aim of ensuring all Queenslanders have equitable access to quality healthcare.
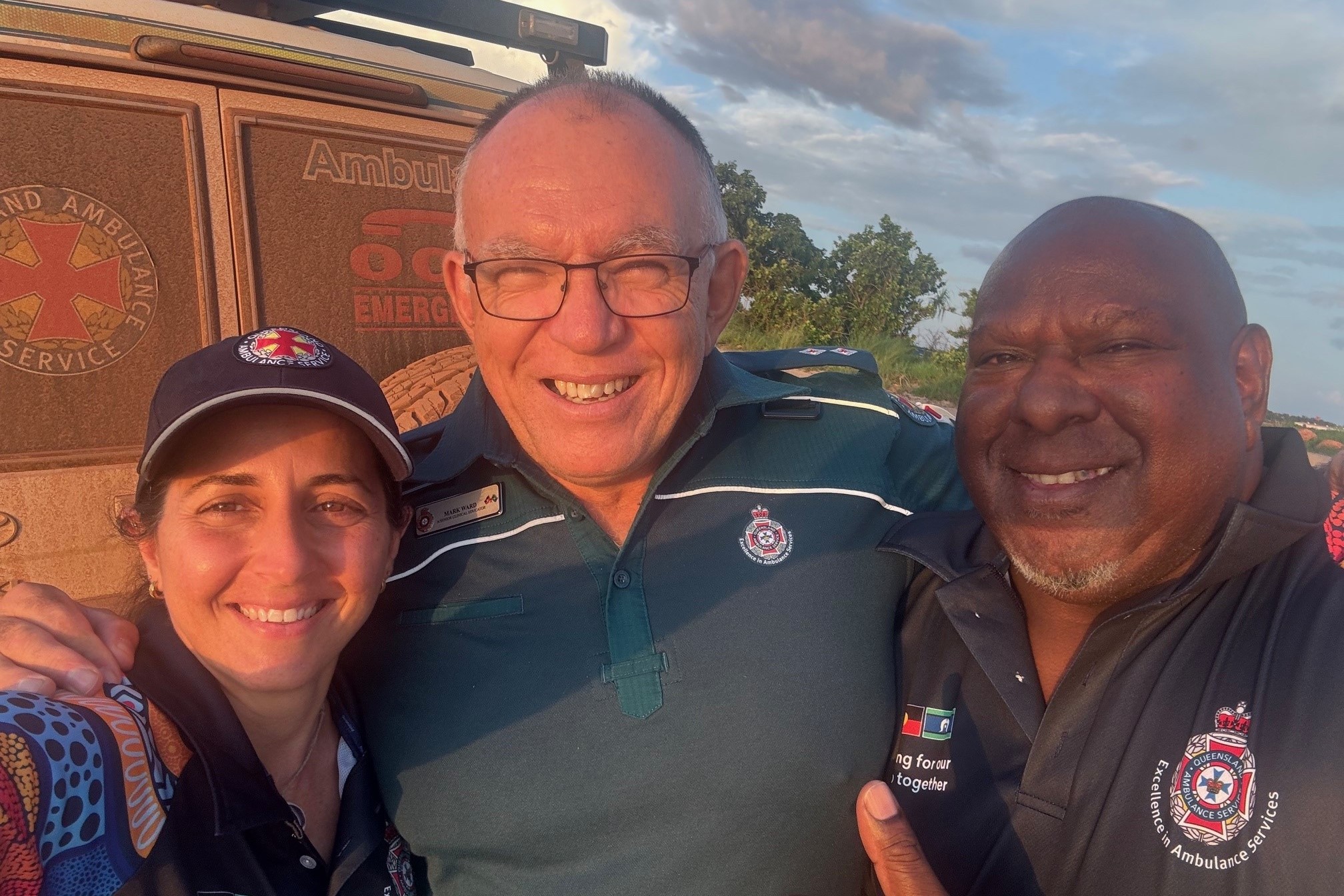
A team of QAS staff in the Far Northern Region then began what would be a long and complex mission to deliver the best healthcare possible to this remote area.
Cape Project Officers Rosie McEachern and Claine Underwood credit Deputy Commissioner North and Rural and Remote Kari Arbouin and Assistant Commissioner Brina Keating with having the foresight recognise gaps in the Cape’s healthcare and being motivated for change.
“Despite QAS having four ambulance stations in the Cape York region and being well serviced by Retrieval Services Queensland (RSQ), vast geographical distances meant there were many small, predominantly Aboriginal communities, which were not being looked after as well as they might be,” Rosie said.
“Further, there was an opportunity to integrate with the Primary Health Centres and Aboriginal community-controlled health organisations to provide a better and more integrated service to these communities.”
But the challenges to deliver better healthcare were many, and often unique, with vast distances, limited infrastructure and accessible road networks, poorer connectivity between towns to health services, higher cost of health services and living, harsh drought or flood-stricken environments, health workforce recruitment and retention, and limited accommodation to name a few.
Rosie said the team decided on a highly collaborative approach to best meet the many and diverse local communities’ needs.
“Extensive consultation has taken place within each community, and this will continue, to ensure the model aligns with local needs, increasing community support and sustainability.

“Our key stakeholders, including community councils and groups, health organisations, government agencies like Queensland Health, Apunipima, and PCYC have been actively involved.”.
Rosie said this initiative aims for a tailored, community-based solution targeted at improving health outcomes in remote communities.
“The Cape York Project is truly unique, investing time and resources to understand local needs in a culturally sensitive way, and assess with intent to improve current health literacy as a platform for enabling community resilience and growth.
“QAS is investing in better understanding the needs of Aboriginal and Torres Strait Islander communities through genuine partnership and authentic conversations. “The Cape York Project team travel to, learn from and work with community to create a purpose-built model of care that is sustainable and transferable to meet their needs,” Rosie said.
“Most community visits are in conjunction with Queensland Health, in addition to working with Torres and Cape Health and Hospital Services (TCHHS), to access grass roots feedback and community investment.
“However, it’s how we maintain, foster and encourage relationships on and off Country that will determine success in both the short and long term.” Rosie said.
There will be five new health-based ambulances (HBAs) in addition to the 22 already in operation across the State.
These will be stationed in Aurukun, Lockhart River, Kowanyama, Hopevale and Mapoon, with expansion in Phase 2 to include Wujal Wujal, Pormpuraaw and Laura.
Rosie said these ambulances’ service areas will extend to include the surrounding community outstations and homelands. >
>
“The HBA model of care is an example of health integration, supporting local communities and health care professionals with resources, education and providing the link to our Clinical Hub and Retrieval Services Queensland (RSQ),” Rosie explained.
The enhancements will include the OIC Field Paramedic role which is a redevelopment of the current Field Officer role previously only based in Kowanyama, Cooktown and Weipa.
This role has now been extended to include Bamaga, , Aurukun and Lockhart River.
Claine said the role focuses on community engagement and education as well as clinical operations that support current health services provided by the Primary Health Care Clinics (PHCC) located in these communities.
“They will also play a huge role in community resilience by teaching our awareness programs, like CPRA, Stop the Bleed, Snakes Alive, Infant/Young Child First Aid Awareness, Mental Fitness to name a few.” Claine said.
“This is a registered paramedic position, where they will be active in their communities and maintain their skills to assist the clinics when required. It’s exciting times, these positions are now open."
Rosie explained there will also be opportunities for Indigenous Cadet Paramedics, once we have our initial Field Paramedics embedded and operational in the Cape.
“Initiatives such as the QAS Scholarship Program and The Indigenous Paramedic Program (IPP) provide opportunities that support both education and employment for Aboriginal and Torres Strait Islander peoples," Rosie said.
The Cape York project reflects the QAS Statement of Commitment to Aboriginal and Torres Strait Islander peoples which reaffirms working in partnership to deliver sustainable health and wellbeing outcomes for our communities in the Cape York region.
This project will be ongoing, and these culturally appropriate conversations will continue.
“The commitment to informed service delivery and greater health footprint through culturally connected care and health integration will ensure contemporary feedback and redesigning of culturally appropriate care across Cape York,” Rosie said.

